IVL
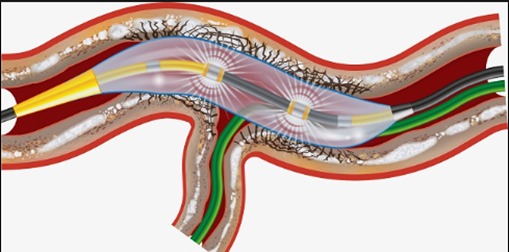
Calcified lesions often mean percutaneous intervention results are suboptimal and increase the risk of procedural complications and future adverse events. Available plaque-modifying devices rely on tissue compression or debulking, with the intention of fracturing calcium and facilitating optimal stent deployment. In contrast, coronary intravascular lithotripsy delivers unfocused, circumferential, pulsatile mechanical energy to safely disrupt the calcium within the target lesion.
The amount of coronary artery calcification increases with age and the presence of cardiovascular risk factors and comorbidities. Up to 20% of percutaneous coronary intervention (PCI) procedures are challenged by severe calcifications, and coronary calcifications have been shown to be an independent predictor of PCI failure and future adverse cardiac events.
Lesion calcification increases procedural complexity and time. More specifically, calcium localisation (superficial or deep), distribution (focal, circumferential and longitudinal extension) and thickness influence procedural success, stent delivery and deployment.